Antibody-drug conjugates (ADCs) mark a significant breakthrough in cancer therapy. These innovative treatments combine the precision of monoclonal antibodies with the potency of cytotoxic drugs, enabling targeted destruction of cancer cells while sparing healthy tissue. By recognizing specific antigens on cancer cells, ADCs deliver their toxic payloads directly where needed, reducing side effects common in traditional chemotherapy. This targeted mechanism opens promising avenues in oncology, offering hope for more effective and tolerable treatments. As research advances, understanding how ADCs work—their components, mechanisms, benefits, and limitations—is essential. This blog explores the science and potential of ADCs in modern cancer treatment.
Understanding Antibody-Drug Conjugates (ADCs)
What Does ADC Stand For?
ADCs stand for antibody-drug conjugates. These are targeted cancer therapies combining an antibody specific to cancer cell markers with a cytotoxic drug. This combination ensures that the lethal drug specifically affects cancer cells, reducing damage to healthy cells. ADCs are under continuous development and refinement to enhance their effectiveness and minimize side effects.
The Evolution of ADCs in Oncology
The journey of ADCs in oncology began with the idea of harnessing the targeting capabilities of antibodies. Over the years, researchers have made significant advancements in this field. Initial challenges included ensuring the stability of the conjugate and effective drug delivery. However, modern ADCs overcome these hurdles with refined design and technology, leading to more approved treatments and ongoing clinical trials aimed at broadening their therapeutic use.
Examples of Approved ADC Drugs
Prominent ADCs on the market include ado-trastuzumab emtansine (Kadcyla) for HER2-positive breast cancer and brentuximab vedotin (Adcetris) for Hodgkin lymphoma and systemic anaplastic large cell lymphoma. These drugs exemplify the success of ADCs in providing targeted cancer treatments, illustrating their potential and setting the stage for future developments in oncology.
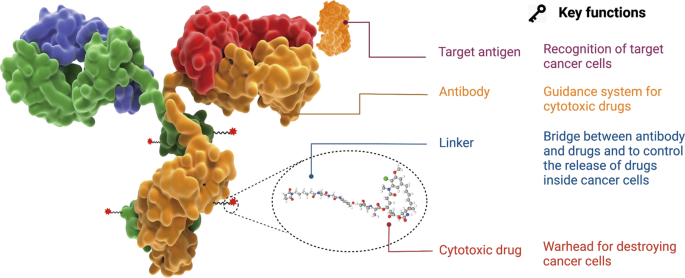
Key Components of ADCs: Antibody, Linker, and Payload
Monoclonal Antibody: The Targeting Tool
At the core of an ADC’s functionality is the monoclonal antibody. It is designed to specifically recognize and bind to antigens on the cancer cell’s surface. This ensures that the drug conjugate homes in on malignant cells, offering a high precision approach to therapy. The specificity of this targeting tool reduces the risk of affecting non-cancerous cells, a significant advantage over non-targeted therapies.
Linker Stability and Drug Release Control
The effectiveness of an ADC hinges on its linker, a chemical bridge that connects the antibody to the cytotoxic drug. The linker must remain stable in the bloodstream to prevent premature drug release. Simultaneously, it must allow swift release once inside the cancer cell. Linker technology improvement remains a crucial research area, ensuring therapeutic efficacy while minimizing side effects.
Cytotoxic Payload: Precision-Driven Cell Killers
The payload in ADCs is a cytotoxic agent designed to kill cancer cells upon release. Commonly, these are potent chemotherapy drugs that, when delivered directly into the target cell, disrupt cellular functions and lead to cell death. The precision in targeting ensures that these powerful agents devastate cancer cells while sparing healthy tissue, highlighting the precision-driven nature of ADC therapy.
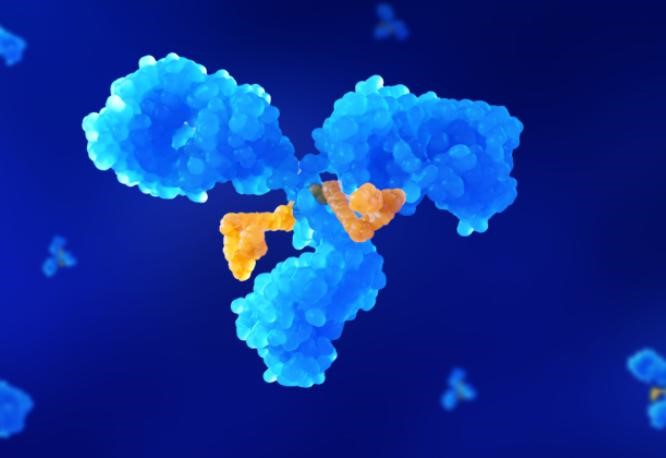
Mechanism of Action: How ADCs Target Cancer Cells
Step 1: Antibody Binds to Cancer Cell Antigen
Antibody-drug conjugates (ADCs) initiate their action by selectively binding to specific antigens on cancer cell surfaces. This targeted attachment ensures the cytotoxic drug is delivered precisely where needed, limiting exposure to healthy cells. By exploiting tumor-specific markers, ADCs reduce systemic toxicity and enhance therapeutic efficacy, representing a precise and effective strategy in cancer treatment.
Step 2: ADC Internalization and Drug Release
After binding to the cancer cell’s antigen, the ADC is internalized via endocytosis. Inside the cell, it is processed to release the cytotoxic drug. This release mechanism is critical, as it ensures the therapeutic payload reaches its target effectively. The overall success of the antibody-drug conjugate (ADC) hinges on the precision and efficiency of this delivery process.
Step 3: Payload Disrupts Cancer Cell Function
The payload’s activation within the cancer cell marks the final stage. The cytotoxic agent interferes with critical cellular functions, ultimately triggering cell death. By precisely delivering the toxic payload inside the cancer cell, the antibody-drug conjugate (ADC) ensures targeted treatment. This approach maximizes therapeutic effectiveness while significantly reducing collateral damage to healthy, non-cancerous tissues in the surrounding area.

Advantages and Challenges of ADC Therapy
Benefits: Precision and Reduced Side Effects
Antibody-drug conjugates (ADCs) offer a major advantage by precisely targeting cancer cells, significantly reducing harm to healthy tissues. This selective approach minimizes side effects common with traditional therapies, enhancing patient comfort and treatment tolerance. As a result, patients often experience better outcomes and an improved quality of life during their cancer journey.
Limitations: Resistance, Toxicity, and Cost
Despite their promise, ADCs face hurdles such as cancer cell resistance, off-target toxicities, and high manufacturing costs. These challenges underscore the need for continuous innovation to improve therapeutic precision, reduce adverse effects, and enhance production efficiency—ensuring broader access and sustained efficacy in cancer treatment.
Innovations from WuXi AppTec’s ADC Series
WuXi AppTec is at the forefront of ADC innovation, advancing drug-linker technologies and refining antibody specificity. Their next-gen ADC platforms address current challenges, such as stability and off-target toxicity. These improvements are crucial for broadening the therapeutic window of ADCs and enabling more effective, targeted treatments across a wider range of cancers.
Conclusion
Antibody-drug conjugates represent a revolutionary advancement in the fight against cancer, offering targeted therapy with precision and reduced side effects. As part of the evolving adc series, these therapies are continually refined to enhance efficacy and safety. While they continue to evolve, overcoming challenges such as resistance, toxicity, and cost remains crucial. Through continuous innovation and research, ADCs hold promise for becoming a cornerstone in cancer therapy, providing patients with more effective and less intrusive treatment options.